
Experiences Gained in a Thirty-Year Study of Prematurely Born Infants
Pediatrics 11(5):425-434, May, 1953
 |
|
If I were to discuss with you the general subject of the premature infant, I would probably bring you little that is new since most of us have gained similar results through our experiences. However, our greatest contribution lies in the fact that we are presenting a long range life history of our smallest graduates in a broad review of the results to date, leaving a more detailed description of the individual infants for future publication.
Much has been accomplished in our time in lowering mortality and morbidity among premature infants but it must be remembered that in these small infants, even with the best of nursing care and most modern equipment, the death rate cannot be cut beyond an irreducible minimum, largely because of their immature development at birth. I am sure it is obvious to all of us that, if we are going to reduce the number of premature deaths, our hope lies in the first week and especially in the first hours of life of these babies. In the general hospital this will require cooperation between the obstetrician, the pediatrician and the nursing supervisors of the two departments.
Our Premature Infant Station was started in 1922 with a capacity of eight cribs, the objective being to provide care for premature infants born in homes or in hospitals not equipped with the necessities for their complete care. The activities of the station have been made possible through the financial assistance and endowment of the Infants Aid Society of Chicago. This group of some 1000 philanthropically inclined women has furnished special equipment and layettes to our station, has founded and equipped a 12-crib-capacity station at the Mt. Sinai Hospital in Chicago, and has, through the years, furnished much in the way of layettes to the Premature Station at Cook County Hospital. The Sarah Morris Hospital Station was established as a memorial to the Society's first president, Hortense Schoen Joseph.
During the first three years of its existence, our Premature Infant Station with its eight cribs admitted only 94 infants due, in part, to the lack of enthusiasm with which the station was accepted by the medical profession in Chicago. Later its capacity was increased to 25 beds, and in 1951 a new unit was developed with capacity for 40 infants (Fig. 1). As might be expected, with a background of years of experience in the care of the premature infant, changes have developed in technics and physical lay-out in such a unit, some of which might be of interest to you. For instance, the hospital has eliminated the requirements for nurses and other personnel in the station to wear masks, while physicians and others who must be in the nursery for only short periods of time are usually required to wear masks. Also, on the basis of experience in our station, it is believed that the standards of the United State Public Health Service for at least 24 and preferably 30 square feet of space per bassinet are needlessly large and that there is a definite operating advantage in the restriction of space per bassinet. The new unit, therefore, has 40 bassinets with a net floor space of 18 square feet per bassinet, which allows for more adequate, detailed supervision from a central control point (Figs. 2 and 3). [See: Black, J. T., "New premature nursery at Michael Reese Hospital," Hospitals 26:83, 1952.]
Chart 1 bears out my previous statement that it is the first few hours of life of these small infants that are so important if we are to reduce our mortality and morbidity statistics.
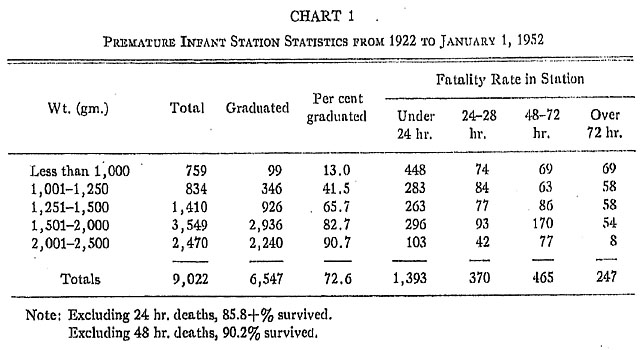
Many of these babies were received late and in poor condition but, by regulation of the Chicago Board of Health, any infant showing signs of life when received in the station must be included in the statistics. In the total group of 9022 infants admitted to the station are included 759 whose birth weights ranged from 605 gm. (Fig. 4) to 1000 gm.; 99 (13.0%) of these smallest infants were graduated from the station and the time of death of the remaining 660 was as follows:
| First 24 hours | 448 |
| 24 to 48 hours | 74 |
| 48 to 72 hours | 69 |
| After 72 hours | 69 |
In the next birth-weight group, 1001 to 1250 gms., 834 infants were admitted to and 346 (or 41.5%) were graduated from the station. Death of the remaining 488 occurred as follows:
| First 24 hours | 283 |
| 24 to 48 hours | 84 |
| 48 to 72 hours | 63 |
| After 72 hours | 58 |
Further study of chart 1 reveals that 99 infants graduated whose birth weights were less than 1000 gm. and 346 infants graduated whose birth weights were between 1001 and 1250 gm. It is this group of 445 prematurely born infants with birth weights of 1250 gm. or less about which I wish to devote most of my remarks today, The 1250 gm. weight as the upper limit for the group of smallest infants was selected arbitrarily for this report. In a. 1949 report we included 20 infants with birth weights between 1250 and 1260 gm. but to simplify a comparison of results obtained in other clinics we are now dividing the birth weights into groups of 250 gm.
One frequently reads in the public press of the birth of one of these small infants and occasionally its early progress is reported but usually its ultimate development is left to the imagination,. This, together with the fact that we must all answer the question of whether these very small premature infants are worth saving, encouraged us to believe that a long range study of our smallest babies would be of instructive interest. We are, therefore, presenting the life history of these infants with as true an estimation as possible of their physical growth and mental development.
Of these 445 smallest infants, 370 are still living and are known to us; their ages range from somewhat less than one to over 28 years, and 335 of them were brought to us for personal interview and photograph and many of them for repeated examination and study; 35, located in distant cities, were examined by their own pediatrician or family doctor who transmitted to us reports of their mental and physical development. Of the remaining 75, we have positive knowledge of 45 deaths but we have been unable up to the present time to obtain positive information concerning the last 30, some of whom may have died. The results of this study are presented in the charts 2-8.
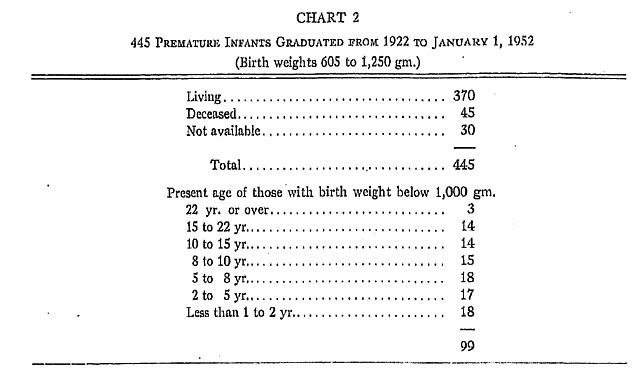

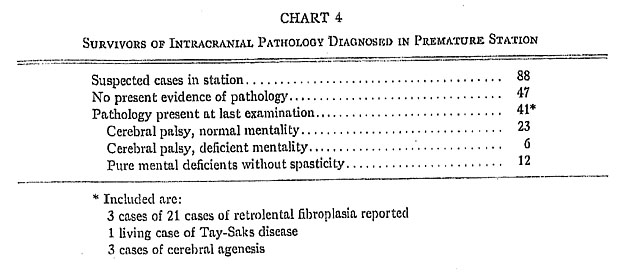
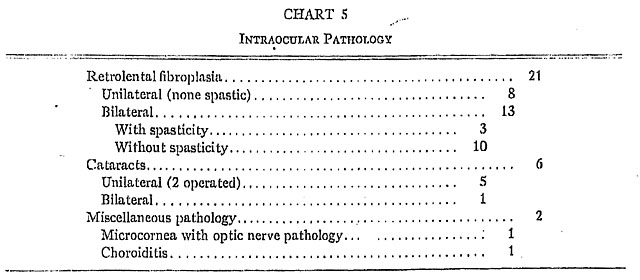
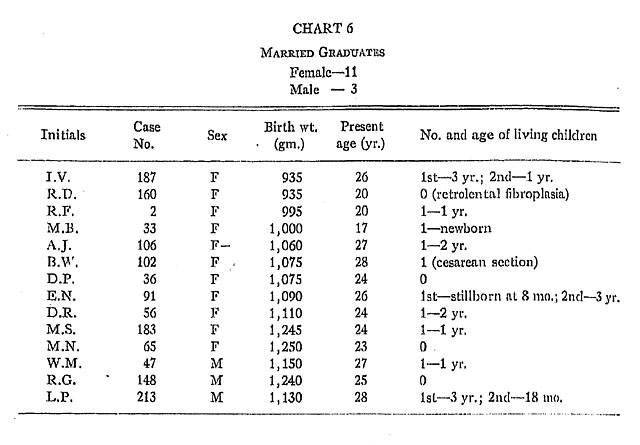
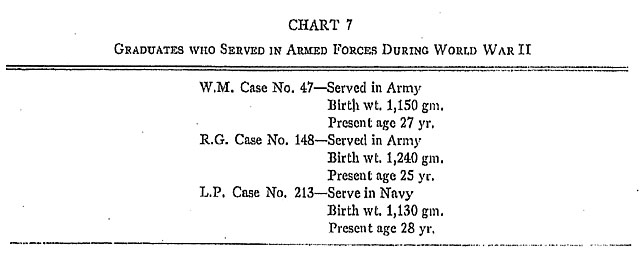
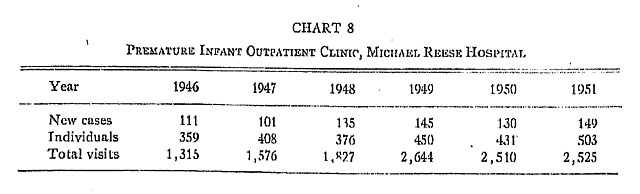
Chart 6 is of particular interest to us for two reasons: (1) for many years it was our custom to give blood intramuscularly at least once to all premature infants in an effort to increase their antibody production and improve their nutritional status. However, in recent years it has been suggested that such administration would result in Rh-negative blood with resultant erythroblastosis. This has not been verified so far as the married females in our series is concerned. (2) Over the years there has been definite skepticism in the minds of some as to the ability of these small infants, first, to become pregnant, and second, to deliver full-term children. Our statistics show that of the 14 graduates who have married (Fig. 5), 10 have been delivered of 12 living children; in only one instance was there a stillborn reported and this graduate later was delivered of a full-term baby.
At the Michael Reese Hospital an outpatient clinic is maintained for instruction of mothers of premature infants and for the care and supervision of graduates from the station. This clinic was established so that the many patients who come from families in the lower income bracket and who frequently do not have private physicians may still have access to guidance in the care of these infants.
I spoke earlier of the fact that some changes have been made recently in the technics used in our new station but I think emphasis should be placed on one practice that has not changed: We are just as firmly of the opinion now as we were in 1922 that breast milk is essential to the welfare of these small prematurely born infants. The mothers of the babies who are patients in the station express their milk at home and send it to the hospital to be used or, if this is not possible, breast milk is obtained from wet nurses and visiting mothers. More than 50% of the breast milk used for our small infants is obtained from mothers who have infants in the station. Except in cases where the mother still has ample breast milk at the time of discharge of the infant, the babies are started on a formula during their last days in the station.
In summary, I would point out that 445 infants weighing 1250 gm. or less at birth have been graduated from our Premature Infant Station during the past 30 years and that approximately 83% are known to us to be still living; that 85% of these living graduates are of average or above average physical development and 90% are of average or above average mental development; three of the young men served with credit in the Armed Forces of our country during World War II, and the 14 married graduates have to date furnished 12 living children to the next generation. I give you these statistics in support of our original belief that any effort expended in ,the care of these smallest prematurely born infants is of inestimable value. Nature has been kind to many who did not survive the ordeals of the early days, but it is hoped that with further progress in their care there will result not only continued lowering of early mortality but improved physical growth and mental development of the prematurely born infant.
It must be evident to all that in order to present such a report as has been given today, many individuals must have been interested in the welfare of these children. Special mention should be made of Evelyn Lundeen's 28 years as Head of the Premature Infant Station, Roberta Stannard's 22 years as Head of the Field Service and Outpatient Clinic, and Winifred Witz's 14 years as second-in-charge of the Station. Many members of the Infants Aid Society have served for long periods in the outpatient clinics and have been of further help in the field services. Credit is also due to members of the Sarah Morris Hospital pediatric staff and resident staff who have served in the station throughout the years.
104 South Michigan Avenue.
From the Sarah Morris Hospital of the Michael Reese Hospital, Chicago.
Borden Award Address read at the Annual Meeting of the American Academy of Pediatrics, Chicago, Oct. 22, 1952.
(Received for publication Oct. 24, 1952.)