Careers in Neonatology

Information for Students and Teachers
Many students and teachers write to “Neonatology on the Web” asking for information about a career in neonatology. We have assembled answers to some common questions here for your convenience. These are, for the most part, only opinions or estimates, and should not be construed to represent the “official” viewpoint of the American Academy of Pediatrics or any other organized medical society or government agency.
What Is Neonatology Anyway?
Neonatology is the medical specialty of taking care of newborn babies, sick babies, and premature babies.
The word “neonatology” is stuck together from several root words and basically means “science of the newborn” — “neo” = new, “natal” = birth, “ology” = science of.
A neonatologist is a doctor that specializes in the field of neonatology. So… “Neonatologist” is basically a fancy technical term for “baby doctor.”
The American Academy of Pediatrics has a nice historical perspective of neonatology at: AAP Historical Perspectives
What Is a Neonatal Intensive Care Unit?
A Neonatal Intensive Care Unit (NICU) is a special area of the hospital that is devoted to the care of critically ill babies. Typically a NICU is completely separated from the nursery for healthy newborns, and may not even be in the same building (the nursery is always located near the rooms for the mothers). The staff for the NICU and the staff for the newborn nursery are completely separate as well.
In most hospitals, babies are only admitted to the NICU directly from the delivery room, the newborn nursery, or from another hospital’s NICU or nursery. For reasons of infection control, if a baby has gone home and then gotten sick and come back to the hospital, the baby will probably be admitted to a pediatric ward or pediatric intensive care unit rather than the NICU. Of course, exceptions can be made if the baby has a problem that definitely requires the constant attention of a neonatologist.
Babies usually stay in the NICU until they are ready to go home, even if that takes several months. This is much different than an adult or pediatric intensive care unit, where the patient will leave the unit as soon as they are stable and do not need help with their breathing and constant monitoring. For this reason, NICUs are often divided by walls or partitions into several distinct regions: a true “intensive care” area where the nurses and doctors spend most of their time at the babies’ bedsides, an “intermediate care” area for babies that are still on IVs or extra oxygen, and a quieter area for the “growers.”
A census of NICUs in 2021 found that there were 1,424 NICUs and 35,601 NICU beds (5,592 level II, 20,631 level III, 9,378 level IV) in the US. (Journal of Perinatology 43:796-805, 2023).
What Kinds Of Problems Do Babies Have?
In most neonatal intensive care units, about half of the babies that are admitted to the unit are full-term babies (born after 37 weeks) and the other half are premature babies — babies that were born too early (before 37 weeks gestation).
Premature babies are not really “sick” — at least, not when they are first born. So why do they need to be in an intensive care unit? It’s because the various systems and organs of their body are not yet fully developed, which can lead to a host of problems that require expert interventions and constant monitoring. For example:
- The lungs are not fully developed, so premature babies may need extra oxygen and/or may need assistance with their breathing from a ventilator (“respirator”).
- The surface area of a premature infant’s body is large compared to its volume and there is very little body fat, so premature babies get cold easily and must be kept in an incubator or radiant warmer.
- The liver is not fully developed, so premature babies have a tendency to become much more jaundiced than a full-term baby. If the jaundice is too severe, and is not dealt with, it can cause brain damage.
- The immune system is not fully developed, so premature babies are very susceptible to infections.
- The stomach and intestines are not fully developed, so many premature babies’ digestive systems cannot handle breast milk or formula adequately, and must get part or all of their nutrition through an IV for a while.
- The brain is not fully developed, so many premature babies don’t breath regularly and reliably on their own without assistance, or can’t suck, swallow, and breath in a coordinated fashion without choking.
- Twins are frequently premature and end up in the NICU, triplets and quads (and more) are almost always very premature and end up in the NICU, with some or all of the problems already listed above.
The problems of the full-term babies that come to the neonatal intensive care unit are typically much different than those of the premature babies, and in some ways are much more complicated and less predictable. Here are a few examples:
- Perinatal asphyxia — a lack of oxygen during the birth process leading to multiple problems such as seizures, kidney failure, heart failure, and so on.
- Congenital defects or “birth defects” — abnormalities of development, such as congenital heart defects, brain malformations, or gastrointestinal malformations.
- Pneumonia, meningitis, or generalized infections in the blood (“sepsis”) — either acquired before birth or shortly afterwards.
- Hereditary or genetic disorders of various kinds — some involve broken or abnormal numbers of chromosomes, others are caused by small mutations in the DNA resulting in abnormal proteins or development.
- Hyperbilirubinemia — if a term baby has certain types of blood disorders, has an infection, or if the mother’s immune system makes antibodies against the baby’s blood type, the jaundice can be very severe and this requires expert attention to prevent brain damage.
- Injuries during the birth process or during the newborn period.
How Many Sick Babies Are There?
The number of babies needing a neonatologist and a neonatal intensive care unit varies quite a bit from one hospital to another. In small community hospitals, the number of sick babies is very small, because obstetricians will send a mother to a large medical center for the delivery if they are anticipating that the baby will have problems requiring special attention.
At Cedars-Sinai Medical Center (CSMC) in Los Angeles, there are about 6000 to 7000 deliveries a year. Most of the babies go to the well-baby nursery so they can be near their mothers, but about 600 of the babies per year (or 10% of the deliveries) have some problem requiring admission to the neonatal intensive care unit (NICU). This is a higher proportion of the deliveries than you would find in a smaller community hospital, because community obstetricians tend to send mothers with high risk conditions to large centers like Cedars-SInai for delivery.
The CSMC NICU has 45 beds. At any given time, 8-15 of the babies in the NICU are critically ill, and the rest are being treated for hyperbilirunemia, recovering from infections or surgery, or are premature babies that are doing well and are just waiting to grow big enough to go home.
Who Else Takes Care Of The Sick Babies?
Aside from neonatology, there are many other careers that involve the care of sick babies. In fact, for almost every kind of patient care role in a hospital, there is a specialized position for people that have extra training in the care of newborns. For example:
- Neonatal nurse practitioners
- Neonatal staff nurses
- Neonatal respiratory therapists
- Neonatal physical therapists
- Neonatal occupational therapists
- Neonatal social workers
- Neonatal nutritionists
All of these people play a vital role in caring for the sick babies and their parents. Pediatric residents and neonatology fellows (neonatologists in training) may also work in the NICU as part of their experience.
How many people does it take to keep a neonatal intensive care unit running around the clock, 7 days a week? Again, this varies quite a bit from one hospital to another, depending on whether residents and interns are participating in the babies’ care, how sick the babies are, whether surgery is done on babies at that hospital, and so on. A typical mix might look something like this:
- 8 neonatologists
- 3 neonatal nurse practitioners
- 2 neonatology fellows
- 1 nurse manager
- 1 clinical nurse specialist
- 1 clinical instructor
- 100 staff nurses
- 1 pharmacist
- 8 respiratory therapists
- 2 physical therapists
Other people who come and go include residents on their newborn nursery or NICU rotations, physical and occupational therapists, and nutritionists who visit babies in the NICU as needed.
How Do I Become A Neonatologist?
The educational track to a career in neonatology is a long one:
- High school – 4 years
- College degree – usually 4 years
- Medical school – 4 years
- Pediatric internship and residency – 3 years.
- Neonatology fellowship – 3 years
After you graduate from medical school, you have an “M.D.” degree, but that doesn’t mean you can take care of patients on your own yet, let alone sick babies! [Note: Graduates of osteopathic medical schools, who receive a D.O. degree, can also enter pediatric residencies and neonatology fellowships.]
Before becoming a neonatologist, you must first learn to be general pediatrician. The pediatric training program, or “residency,” is 3 years long and is mostly comprised of time in the clinic, inpatient wards, and emergency department under the guidance of pediatric faculty. The resident takes care of patients in a closely supervised environment, goes to daily lectures and teaching conferences, and works night shifts to handle pediatric emergencies in the hospital. The resident is also exposedto a broad broad range of pediatric subspecialties (including pediatric intensive care and neonatal intensive care) for one or two months at a time.
Pediatricians, for the most part, practice in an office setting and take care of children ranging in age from birth to 18 years. Much of their practice is preventative and educational, but they must also be flexible and knowledgeable about physical, mental, and emotional development and about an extremely wide range of diseases. For more information about a pediatric career, see Consider a Career in Pediatrics on the American Academy of Pediatrics web site.
Once you have finished your pediatric training, you must then take 3 additional years of training called a “neonatology fellowship.” This time is typically divided between taking care of lots of critically ill babies in a neonatal intensive care unit, under the constant supervision of experienced neonatologists, and clinical or basic science research. You will learn to handle the full gamut of neonatal problems and diseases as well as planning, carrying out, and publishing about a research project related to newborn care.
There are several very important exams that you must take along the way that certify you for patient care. These exams are often called “Boards” which is short for “Medical Board Examinations.”
- There is a set of national medical examinations that you take during medical school and internship (the first year of Pediatric residency). After you have successfully completed this series of examinations, you will be licensed to practice medicine in your state.
- There is a set of pediatric board examinations that you will take the year after you finish your pediatric residency. When you successfully complete these exams, you will be certified as a pediatric specialist.
- The last set of exams is taken after you finish your neonatology fellowship. When you pass these exams, you are certified as a subspecialist in neonatal-perinatal medicine.
You will probably say “Gosh! 14 years after I graduate from high school. Forget about it!” Yes, it’s a long time, but it is not as bad as it sounds. You aren’t just sitting in a classroom for 14 years — after the second year of medical school, you spend most of your time taking care of patients under supervision, and after you graduate from medical school you will spend all your time around children. Residency and fellowship are hard work, but they are also fun, and there is always lots to learn and do.
Students occasionally write and ask us about careers in pediatric surgery, particularly newborn cardiac surgery. Pediatric surgery is a demanding and rewarding career, but the training follows a completely different track from pediatricians and neonatologists. For more information, go to “What is a pediatric surgeon?” on the HealthyChildren.org site.
How Many Neonatologists Are There?
According to a workforce report from the American Academy of Pediatrics in October 1996, there were at that time 3688 board-certified and board-eligible neonatologists in the USA. Certification was still relatively new at that time. By 2023, there were 7,871 neonatologists had ever been certified, although 2,552 of those had allowed their certificates to lapse, and information on how many are still actively practicing is hard to come by, as some may not be active in the workforce due to retirement, death, or other factors. It is an aging workforce, over 60% of the certified neonatologists are over 50 years old, nearly 33% are over the age of 60, and the median age is 49 years. Of the currently certified neonatologists in 2023, 58.3% identify as female, and 41.7% identify as male. This represents a significant shift, as more than 75% of neonatologists greater than 60 years of age identify as male.
According a “landscape analysis of neonatal-perinatal fellowship programs” in 2020, there were 98 active fellowship programs in the U.S. Over the years 2005 to 2020, the total number of first-year neonatology fellows increased from 220 to 298, with an increasingly large proportion of women (61% in 2005, 69% in 2020).
Where Do Neonatologists Work?
Many neonatologists work in large hospitals or medical centers as full-time employees, although an increasingly large number work in smaller community hospitals and may provide care at several different hospitals. According to recent survey data, about 1/3 of neonatologists are in academic practices affiliated with training programs and teaching centers, and about 2/3 are in private practice. Many of the neonatologists in private practice work for large companies such as Pediatrix, which staff community NICUs under contract.
In hospitals with an NICU, neonatologists may take charge of a baby’s case immediately based on the baby’s birthweight or condition and hospital policies. For example, most hospitals with NICUs have a policy that says something along the lines of “if the baby is sick enough to need intensive care or is significantly premature, it must be taken care of by the hospital neonatologists.” Neonatologists may also be asked to take responsibility for the care of a baby by that baby’s pediatrician (this process is called “referral”).
Within a typical large hospital setting, a neonatologist’s time is divided between the neonatal intensive care unit (NICU), the well baby nursery, the delivery room, the high risk infant followup clinic, some administrative meetings and educational conferences. In an academic center, neonatologists also devote time to research and to teaching medical students, interns, and residents.
How Much Do Neonatologists Make?
I just knew you were going to get around to this topic sooner or later!
There is no simple answer to the question though. Neonatologist salaries are subject to the law of supply and demand like everything else, and depend on many factors, for example:
- Region of the country (West Coast, New England, NorthWest, Deep South, etc.)
- Years of experience
- Urban or rural setting
- Number and acuity of patients
- Academic center or private hospital
- Amount of in-hospital night call
- Direct patient care vs. supervisory role
- Profit-sharing or other incentive programs
The states with the highest number of neonatologists per 100,000 children as of 2023 are shown in the figure below.
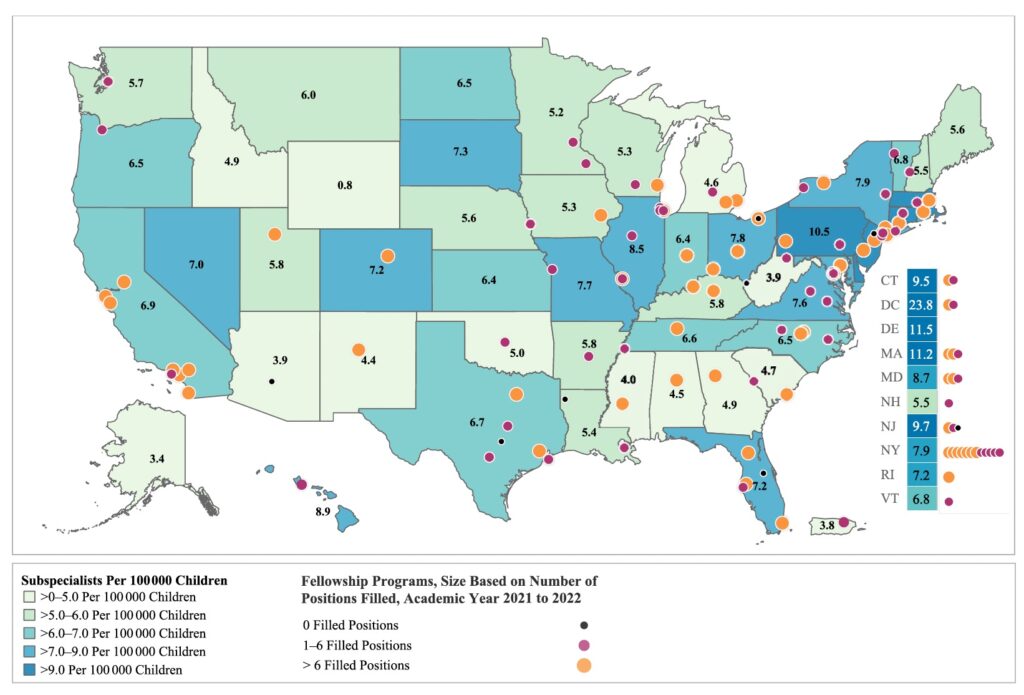
A salary survey in 2018 found a median salary for neonatologists in the U.S. of $268,000, but salaries varied greatly between academic centers, community hospitals, urban and rural environments, as well as by state. The highest salaries in 2023 were found in New York, Vermont, and Caliifornia.
What Do You Like Most About Your Job?
Neonatology is fun because the babies are so resilient! Given the right kind of support, they can snap back from almost anything in an amazingly short time. They are so much smarter and more complicated than most people give them credit for, too. Even a premature baby already has a distinct personality and style when they are born. Some babies are “easy,” some are “irritable,” some are “social,” and this is easily recognized as still being their style years later.
Neonatology is also fun because it’s a “hands-on” kind of job. Although neonatology is an incredibly specialized occupation in one sense, it’s also very generalized. It’s one of the few areas left in medicine where a physician can handle nearly all aspects of the patient’s care, and do lots of “procedures” (IVs and central lines, intubation, thoractostomies, spinal taps, peritoneal taps, etc.), without calling in a flock of consultants.
Neonatology is one of the few remaining medical specialties where you can get to know patients and their families on a day-to-day basis over a fairly long period of time. Very small premature babies may be in the hospital as long as 4-6 months while they get over their initial problems and then grow big enough to go home safely. The doctors, nurses, and parents often form lasting friendships, and the babies come back to visit us as toddlers, students, and even as teenagers!
And last but not least, neonatology is fun because all the other people in an NICU are so great to be around. The doctors and nurses that work in neonatal intensive care units tend to be friendly, kind, even-tempered people that work well as a team and can empathize with sick babies and their parents. And because, after all, it’s an intensive care environment, the doctors and nurses also tend to be smart, experienced, practical people that can think on their feet and take appropriate action quickly when that is necessary.
But… Neonatology is not for everyone. It can be stressful, the hours are long, the pay is not great compared to many other medical specialties with the same (or less) amount of training, and it gets harder and harder to stay up all night in the NICU as you get older. If you are an introspective person that doesn’t like to be pushed around by events, if you tend to get bogged down in details, if you find it hard to work in a team, or even if you just don’t cope well with lack of sleep, you may want to think about doing something else.
View the AAP’s neonatologist career satisfaction survey.
What Does The Future Hold For Neonatology?
There have been many technological advances in neonatology in the last few years, such as the use of surfactant, high frequency ventilators, extra-corporeal membrane oxygenation (ECMO), and nitric oxide. There has also been amazing progress in other, related areas such as cardiac surgery for infants, medical genetics, and heart transplants. Computerization has become pervasive as well, with on-line caregiver documentation, orders, flowsheets, medication administration records, and interfaces to ventilators and monitoring devices. These new technologies and techniques have made it possible for us to save many tiny or critically-ill babies that would have died twenty years ago, and use the rich data from electronic medical records to evaluate outcomes, reduce medication errors, and implement improvements in care.
The place that improvements are desperately needed, though, is in the area of prenatal care. Although it is not very exciting or dramatic, perhaps, it is much healthier for the baby (and much less expensive) to prevent premature birth than to use a lot of exotic technology to save a premature baby after it is born. Unfortunately, we still don’t know why most babies are born prematurely, and our society does not place much emphasis on prenatal care and preventative medicine compared to intensive care. While the survival of premature infants as improved drastically over the last forty years, the percentage of premature deliveries has stayed essentially the same, and recently the percentage of premature births has actually been increasing due to the use of fertility drugs and the widespread abuse of cocaine.
Other Information about Neonatology and NICUs
- Council on Pediatric Subspecialties – Neonatology
- Neonatology Fellowship Programs (ERAS)
- Neonatology Practice Types
- Neonatologist Work Responsibilities (AAP)
- “NICUs in the US: levels of acuity, number of beds, and relationships to population factors”
Created 8/1/99 / Last modified 8/30/2024
Copyright © 1999-2024 Neonatology on the Web / webmaster@neonatology.net
Last Updated on 11/30/24