Equipment in the NICU
A neonatal intensive care unit (NICU) can be a confusing place with lots of complicated-looking electronics, dials, wires, tubes, strange noises, beeps, alarms, buzzers, flashing lights, pressure hoses, and bubbling cannisters that are confusing to visitors and parents. Here is a sampler of the equipment that is commonly seen in an NICU.
 | Radiant warmers are used when a baby is very unstable or extremely premature. Small babies have a large surface area compared to their volume, and little body fat, and cannot maintain their own temperature. The overhead arm contains electric heating elements that are directed down toward the infant. A thermostat is hooked up to a sensor on the baby’s abdomen and adjusts the power of the warmer up and down dynamically so that it delivers whatever heat is necessary to keep the baby at the perfect temperature. The shelves attached to the warmer allow monitors and other equipment to be placed conveniently near to the baby, the glass side walls prevent the baby from being chilled by drafts, and the open nature of the radiant warmer allows physicians and nurses to have easy access to the baby from all sides during the most critical periods. |
 | When a baby is relatively stable but still premature or requiring intravenous fluids or other special attention, he or she is cared for in an “incubator.” The incubator keeps the baby warm with moistened air in a clean environment, and helps to protect the baby from noise, drafts, infection, and excess handling. Incubators were invented in France in the late 1800’s and the earliest incubators were, in fact, modeled after poultry incubators — hence their name. Incubators are sometimes called “isolettes,” but “Isolette” is actually a brand name for a particular company’s incubator product. You’ll see many varieties of incubators in NICUs but whether they are flashy or plain, colorful or austere, they all do basically the same job. |
 | The scale is one of the most humble yet one of the most important pieces of equipment in the NICU. Every feeding, IV solution, and medication is calculated and based on the baby’s weight, and it’s critically important that the weight be accurate, up-to-date, and readily available at all times. It’s part of the morning ritual in every NICU to weigh each baby at the same time and in the same way each day, and then chart the weight on the baby’s flowsheet. The weight is carefully corrected for the weight of the diaper and any equipment that is attached to the baby, as well as the clean piece of paper that the baby lies on during the weighing. It is typically recorded in grams and is accurate to within 5 grams. Note that one pound = 454 grams. |
 | A physiologic monitor, sometimes called a cardiorespiratory monitor, is attached to sensors on the baby and provides a constant read-out of the baby’s heart rate and rhythm, breathing rate, arterial or central venous pressure, and other useful information. Alarms can be configured to provide an alert when any of the vital signs being monitored goes above or below a certain limit. Monitors come in a huge variety of shapes, sizes, configurations, and the most recent models contain embedded computer systems that are capable of filtering out false alarms, recording and reviewing data for extended periods, performing some degree of trend analysis, and many other sophisticated functions. |
 | The pulse oximeter, or “pulse ox,” monitors the oxygen saturation of the baby’s blood. It does this by shining light through the baby’s skin and measuring the color of the light that is transmitted. Most of you are familiar with the concept that red blood is arterial and blue blood is venous; this is another way of saying that blood which is being pumped by the heart from the lungs to the body and has a lot of oxygen in it is red, whereas blood that is returning to the heart through the veins after oxygen has been removed by the body’s tissues is blue. By measuring the transmitted light at certain colors very precisely, the pulse oximeter can provide an estimate of how much oxygen is in the blood. The pulse oximeter can be fooled, however, when the flow of blood to the hands and feet is poor, such as when the baby is cold, or when the baby’s blood pressure is low. |
 | The “Dinamap” takes the baby’s blood pressure at programmed intervals. It inflates a plastic cuff around the baby’s arm or leg, exactly like a nurse or doctor taking a baby’s blood pressure manually. |
 | Infant ventilators (respirators) breath for the baby when the baby is too sick or too weak to breath for itself. There are many different types and brands of ventilators in use in NICUs; the one shown here, the Sechrist 100B, was popular in the 1980’s and is still in common use today. |
 | Recent models of infant ventilators are heavily computerized and support diverse modes of operation, including “assist control.” Some models can provide real-time data on the baby’s pulmonary function. |
 | An “oscillator,” or “high frequency oscillatory ventilator” (HFOV), is a new type of ventilator that came into use in the 1990’s. The equipment shown here is the Sensor-Medics 1000A, a popular brand. Unlike traditional ventilators, which essentially inflate and deflate the baby’s lungs like a set of billows, the oscillator keeps the lungs open with a constant positive end-expiratiory pressure (“PEEP”) and vibrates the air at a very high rate (up to 600 times per second). The vibration helps gases to quickly diffuse in and out of the baby’s airways without the need for the “bellows” action which may damage delicate lung structures. Although oscillators are not appropriate for every disorder and situation, there is no doubt that because of their incredible power, oscillators have made it easeir to care for the very sickest babies with certain types of lung problems. |
 | A “blender” mixes pure oxygen and air (or other gases) in precise ratios and delivers the resulting mixture to the baby. The mixture is adjusted based on the level of oxygen in the baby’s blood, measured by pulse oximeter or blood gas machine. Blenders are typically attached directly to ventilators, but may also be used in a stand-alone configuration — as shown here — when a baby is receiving oxygen during a resuscitation or by face mask or is in an oxygen “hood.” The orange box and water cannister attached about half-way down the pole heat and humidify the gas mixture before it is delivered to the baby. |
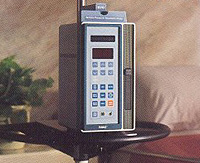 | IV pumps, or infusion pumps, are a crucial item of equipment in an NICU. Most sick babies have one or more intravenous (IV) or arterial lines, and the fluid that is delivered through those lines must be very carefully regulated, all the way down to the amount of 0.1 cc per hour (about 1/30 of a teaspoon per hour). There are many brands, sizes, and shapes of IV pumps; the pump shown here is called an IVAC. |
 | Phototherapy lights, or “bili lights,” are used when babies are jaundiced (yellow). Some degree of jaundice, which is caused by the presence of a molecule called bilirubin in the blood, is common and even normal in newborns. However, in sick infants, jaundice can result from a variety of problems, and when jaundice is extreme it can cause brain damage. During the 1970’s, it was discovered that certain wavelengths of light (in the blue part of the spectrum) can cause a chemical reaction that converts bilirubin into a harmless form as blood passes through the skin. It’s important to note that bili lights do not deliver any ultraviolet light, so the babies are not in any danger of sunburn or other toxic effects. However, as a safety measure, the babies’ eyes are usually shielded with a cloth covering when they are under bili lights. |
 | A drainage pump may be hooked up to a naso-gastric (NG) tube or to other tubes in order to keep secretions from accumulating in the stomach or to drain other areas when the infant is very sick. These pumps can be adjusted to provide constant or intermittent suction. |
 | A blood gas machine analyzes a sample of the baby’s blood, usually obtained from an arterial catheter or from a “heelstick,” and reports the pH and the level of oxygen and carbon dioxide. It also calculates values for the bicarbonate level, oxygen saturation, base deficit, and so on. These values are then used by the neonatologist, nurse practitioner, or respiratory therapist to adjust the setting of the ventilator and the oxygen blender. It was not practical to do blood gas tests on babies until the 1970’s, when simple techniques for umbilical arterial catheterization were developed and blood gas machines appeared that could perform tests on “micro-samples.” Today’s blood gas machines can perform a complete analysis on less then 0.2 cc of blood (less than 1/10 of a teaspoon). |
 | For many years, the “lightbox” was the traditional tool for viewing X-rays. Essentially, it’s just a big metal frame with backlights and a translucent plastic face. X-rays are clipped onto the front of the lightbox and can then be viewed and interpreted by transmitted light. Nowadays, in any large hospital, images are viewed online. However, there are still some lightboxes around and they can be useful when looking at an X-ray that arrives with the baby from an external hospital. |
 | In the modern, digital era, films are read on-line and the images can be manipulated through software to aid interpretation — the contrast and brightness can be manipulated, the image can be flipped or rotated, edges can be enhanced, areas of interest can be enlarged, old images can be retrieved from disk storage and compared with the new images, etc. Most importantly, an image can be viewed in more than one place at a time, the neonatologist does not need to wait for film to be “developed,” and each image is stored and backed up electronically so it cannot be misplaced in the radiology file room or borrowed and lost. |
 | A transport incubator is used when a sick or premature baby is moved from one hospital to another — for example, from a community hospital to a larger medical center that has a neonatal intensive care unit. In fact, a transport incubator is like a little self-contained intensive care unit on wheels. It usually has a miniature ventilator (respirator), cardio-respiratory monitor, IV pump, pulse oximeter, and oxygen supply built right into its frame. A specially-trained physician, nurse, and respiratory therapist typically accompany the baby fhroughout the trip. |
 | A defibrillator is used to “shock” the heart from an abnormal rhythm pattern back into a normal rhythm. Every neonatal ICU has one of these devices, but they are rarely used there. Abnormal heart rhythms are quite unusual in babies, even those babies with several cardiac abnormalities — arrhythmias are more typical of aged patients with damaged heart muscle or conduction pathways. |
Last Updated on 04/23/23