History of Perinatal Medicine – Toubas
History of Perinatal Medicine
by Paul L. Toubas, M.D.
Professor of Pediatrics
University of Oklahoma Health Sciences Center
[Note: This content was originally published at http://hippocrates.ouhsc.edu/Toubas/index.html. It was downloaded on 2/6/2000 and is reposted on Neonatology on the Web because it is no longer available in its original location.]
We are presenting work in progress, thus incomplete and subject to additions and corrections. The relation between the different actors of scientific medical progress is still actively studied.
Most of these physicians have been forgotten, but we have attempted to revive them so that they can participate in our activities and give us the sense of belonging to a common family of knowledge. Understanding the past is understanding the future.
This web page is specially dedicated to the pediatric residents and fellows of our universities. The present knowledge of Pediatrics has been transmitted and improved for generations. They belong to a great family.
Introduction of Pierre Budin,
one of the fathers of modern Perinatology
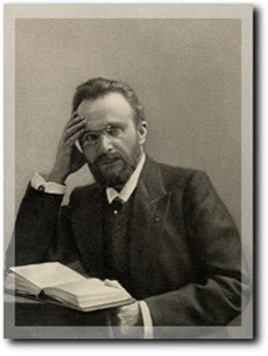
Dr. Toubas has been interested by Pierre Budin since 1974. His attention was attracted by the few mentions of Budin’s work in neonatology textbooks. Further research on Pierre Budin (his name was attached to five different wards in the Assistance Publique hospitals in Paris) came to a dead-end. In 1980, when Dr. Toubas moved to the United States, he left a note with an antique book dealer (Librairie Alain Brieux) in Paris to alert him if anything about Budin became available. Ten years later (in 1991) this bookstore, specializing in antique books, wrote that the personal archives of Pr. Budin were available. Dr. Toubas purchased them at once for about 600 US dollars. He initially did not plan to study the 40 pound stack of documents in great detail, but cursory study revealed the great historical interest of the collection and he was invited to make a presentation for the Perinatal Association from the American Academy of Pediatrics in Denver (May 1992). Since then, interest in Pierre Budin and others has increased in the United States and in France and more presentations of the life and work of Pierre Budin and collaborators have been scheduled.
Pierre Budin, along with Tarnier, is the father of modern Perinatology. Lacking full documentation on Budin, some authors have attributed to him the invention of the incubator (1). In fact, his mentor, Tarnier, was the first to apply the egg incubator to weakling infants (7,11,12,13). The role of Budin, however, goes beyond the application of rescue technology to the newborn infant. Budin was the first obstetrician who realized that his role should not be limited to the care of pregnancy, the minimization of complications of delivery and the extraction of the fetus (14,15). Budin understood the importance of data gathering and analysis (a skill he had obtained from helping his father to manage the huge farming property of the Budins) in order to direct action (14,140 ). Budin focused his interest on infant mortality rates and, with logic, attacked its roots. He led the way in insuring normal growth and nutrition for the infant by educating the mothers in preventing one of the most deadly complications of infancy (at the end of the 19th century), infantile diarrhea (153). Physicians of this period were not interested in the infant until two years of age. The obstetrician (an emerging specialist) thus took charge of mother and infant (14,15,16,17). Success in decreasing both maternal and infantile mortality are reflected in a lecture given in 1900 (14).
Budin was also an influential physician. He had contacts with members of the French government. France, at the end of the 19th century, combined low birth rate and high infantile mortality. This led to the fear that the young French republic would be dwarfed and overwhelmed by Germany. The combination forced French authorities to invest simultaneously in both the development of a very modern-for- the- times system of health care for pregnant women, and a very efficient educational system (18). There was also a tremendous need of men to colonize Africa and East Asia since raw materials were needed for the industrialization of France. Great Britain, already industrialized, exerted an intensive economical pressure on France. Budin (a member of the hygiene society [14]) was deeply involved in the execution of the health care programs. The French saw very clearly that their best investment for the future was healthy, educated children. Their enterprise was very successful. By a tragic irony, however, numerous male children who Budin saved from dying of diarrhea and dehydration during their first year, fell on the battle fields of the first world war. Budin only postponed the death of these infants. They died as healthy adolescents, but perhaps after influencing the course of history. The French fear of depopulation (18) led ultimately to the loss of 1,500,000 lives (not counting the wounded and handicapped) during the four years of the war.
The history of Pierre Budin placed into the socio-political and scientific context of his days is a lesson which is still valid. Neonatology is a new subspecialty in Pediatrics. It emerged in the early forties, but the interest in actively rescuing premature infants dates from the time of Budin. It was further energized by the 1962 death of Patrick Bouvier Kennedy, the premature son of President John F. Kennedy and his wife Jacqueline. This specialty of Pediatrics has made very rapid technological progress helping to rescue many infants. The physicians of our century, too preoccupied by technological advances, have found themselves entangled in intense ethical issues. Finding and understanding the roots of this discipline has become a must. The papers of Budin also speak to our ethical conundrum today.
There is not enough material in English on Budin. Our discovery of the personal archives of Pierre Budin will help clarify the march of ideas in the area of obstetrics, pediatrics, and epidemiology at the turn of the 20 th Century.
Biography – Forgotten lessons of the past –
The biography of Dr. Pierre Budin
The history of medicine should have a more important place in the education of medical students. Neglecting history is like erasing memory. Ignoring the past is destroying an important part of science, which is past experience. Neglect of history represents a lack of respect for our roots and leads to identity crises. History is the necessary ingredient for future experiments. This is the story of Pierre Budin , the first perinatologist.
Pierre Budin had published books and articles which can easily be found in medical literature. The recent discovery of his personal archives has helped considerably in understanding the character, goals and achievements of Dr Budin, who is recognized as the father of the “clinics for nurslings”. These clinics contributed to the marked decline in infant mortality at the beginning of this century and led to pediatric preventive care.
Childhood 1846-1864
Pierre Constant Budin was born in 1846at Enancourt-le-Sec, en Vexin, a very small village in the northwest part of France. The son of farmers (5) he attended grade school at the College of Beauvais located in an old Capucins convent, “where in Budin’s wards our parents, more concerned with our future than with our personal aspirations, had imprisoned our childhood” (1). The old college had thick walls “dripping sadness and boredom” and “the heavy door of the college closed on us with a noise which echoed painfully in our children’s heart”. In this institution, Budin’s friend Gallipe who remembered Pierre as “alert, lively, with a touch of teasing in the eyes.” He was constantly well groomed. Pierre did not fight, but “was tenacious and courageous if attacked” (1). Unfairness revolted him. Pierre was a good student , “bringing in his daily work order, accuracy and neatness.” He already had a regular , very small and somehow feminine handwriting. According to his friend, he already combined a strong character with charm, gentleness and happiness, in other words, “the gift to please, bind and retain.”
Pierre Budin describes his time in school as a “painful memory.” Thinking about it, he said “gives me chills up in my spine; I have been so stressed by it that for a while, one of my nightmares was that my family brought me back to the college of Beauvais.” Pierre, in one of his speeches forty years later, remembered a little room, “le petit local,” where students were punished by being confined, sleeping on wooden floors and engraving their names in by the window frame, like prisoners in a jail. “Some teachers brought unjust punishments on some students and we revolted”, Budin said, but “we already had critical minds (l’esprit critique) and did not want to always accept everything we were told as truth.” “At night, when all our comrades went back to bed, when we were left thinking in the dark about a bad night’s sleep, spent on the hard floor, we heard very light footsteps. A key opened the lock without noise. Lantern in hand, a tall, thin 27 or 28-year old young lady came in (we were about 12 years old ourselves!). She was the daughter of the principal; she gently reprimanded us about our conduct, tried to make us promise to be well behaved in the future, and finally brought us the pardon of her father. This is the way we first learned about the consoling woman; she was already the image of the “eternal woman.” (1)
The Student 1865-1867
Budin was a bright student at the Lycee Napoleon and obtained a baccalaureate in philosophy. Lionel Laroze one of his schoolmates, indicates that Pierre was near-sighted and frequently importunated by an exchange of poetry written under the table by Richepin and Laroze and illegally transferred over his head. Budin did not write poetry and his friends doubted that he liked it. Despite a lack of artistic creation ,he was judged by his peers as a very good and dedicated man.
Medical School and Residency 1867-1877
Budin started medical school in Paris in 1867. He became a resident in 1872 spending part of his first year of residency at the Maternity Hospital, since from the beginning he had been attracted by obstetrics. When Budin was a resident, Puerperal fever was ravaging maternity wards, so in 1874 he travelled to Edinburg, like his friend Lucas-Championiere, and did a fellowship with Lister to learn antisepsy; then visited the great masters of Obstetrics in England and Germany. Back at the Maternity in 1875 as a fourth-year resident (residency in France is still four years), and worked under the supervision of Dr. Tarnier (the obstetrician who developed a means for using of egg incubators to help sick newborn infants). Dr. Tarnier was already impressed by the work of Lister but instead of phenic acid used sublimate for antisepsis at the maternity. By this time, Budin has found “his path” (2). He would dedicate his professional life to the improvement of maternity wards. At that time , obstetrical beds were part of general medicine wards. Budin requested special services for pregnant women and the creation of the specialty of obstetrics. During his residency period, he published work on obstetrics. The Ligation of the Umbilical Cord was published in the Progres Medical (3).
The Physician – Curbing Maternal Mortality 1876-1892
Budin received his Medical Doctor degree in 1876. His thesis, titled “About Fetal head in Obstetrics, has remained a classic (4). In 1878, he became Chef de Clinique (equivalent to assistant professor) of Pr. Depaul. Promoted associate professor in 1880, Budin was well known for his teaching to medical students, residents and physicians on the art of obstetrics. When the specialty of Obstetrics was finally recognized in France, he competed in 1882 for the position of Obstetrician of the Paris Hospitals. (5). Budin obtained the highest mark on this examination, and was appointed along with Porak, Boissard and Ribemond-Dessaignes. Pierre Budin became the Obstetrician in Chief of the Hospital de la Charite (1882) in which position he modernized the teaching of obstetrics. (6).
The Disease 1885 (5)
The career of Budin was interrupted by serious health problems, which deserve to be reported, because he submitted, for the times, to an experimental surgical treatment.
At age 38 , Budin who had already complained of hepatic crises and was treated without success by his peers, opted for a laparotomy, a rather risky procedure for those times. Pierre himself organized an operating room on his property at Beaulieu sur Mer, a small town on the Mediterranean Sea. The surgeon who performed the surgery was Lawson Tait from Great Britain. French Surgeons from the Faculte de Medecine de Paris were upset and predicted the worse outcome. Pierre was anesthetized with chloroform. Phenic acid was used for disinfection. An hydatic cyst was removed. The surgery was a success and six months later Budin was back to work. During this period, Budin had delegated various parts of his work to his assistants, mainly Crouzat and Maygrier. Crouzat continued to correct the book de L’Obstetrique published under the direction of Tarnier, and Maygrier took care of the teaching (he even lived in the Paris apartment of Budin during this time) and the examinations of the students of the young specialty of Obstetrics. An abundant correspondence between these men documents in great details the support Budin received from his peers and also his courage ( and the courage of his surgeon) in affronting a risky surgery. Some of his colleagues were present in the improvised operating room and one mentions that he had scrubbed his body with turpentine and put on brand new clothes in order to prevent any contamination. Another friend from Montpellier had provided the gauzes ! From this time on, French physicians held British surgeons in great esteem. The Laparotomy technique of Lawson Tait was translated and published.
Creativity
Budin was so convinced of the importance of understanding infection that in 1889 he returned for a course at the Pasteur Institute, and, in the following year sent his assistant Dr. Chavanne to the same course. Concerned by the very high infant mortality rate, Budin founded the first clinic for “nurslings” in 1892 (5,8,9,10). Pediatricians and Obstetricians rapidly realized the importance of industrially sterilized milk but Budin and Soxhlet studied home sterilization of milk (11,12,13). He thought about the smallest details, including the rubber nipple and designed a smaller nipple for low birth weight infants (named “le galactophore”). He also designed an apparatus to pump the breast milk, so that premature infants could benefit from it (“teterelle bi-aspiratrice”).
Budin was not alone in promoting mother’s milk. It is interesting to note that in 1890 , in Nancy, Professor Hergott had created a follow-up clinic and rewarded breast feeding mothers for the their infants weight gains. This practice attracted a lot of women to the maternity of Nancy and greatly increased the number of breast-fed infants.
Budin succeeded Pr. Tarnier in 1895 and became Chairman of Obstetrics at the Port Royal Maternite ( an ex-convent transformed into a maternity) where , after forcing Mrs Henri, the powerful midwife-in-chief to resign, he developed the first specialized infant care center, the pavilion for “weaklings” (5). The latter included infants who were premature and small for gestational age, although it is felt that Budin figured out that there was a difference between the two groups. He became chief in 1898 of the Tarnier Maternity (a state of the art facility for these times) located at rue d’Assas, next to the Luxembourg Garden in Paris.
The Academician
Budin became a member of the French Academy of Medicine in 1889. He belonged to numerous societies: Society of Biology, Anatomical Society, Society of Public Medicine and Hygiene, Society of Legal Medicine and the Obstetrical French Society which he founded in 1898. Very well known in France and in neighboring countries, he was an honorary member of the London Obstetrical Society, the Edinburgh Obstetrical Society and Boston Obstetrical Society. He was also a member of the Italian, Spanish and German obstetrical societies (14,15). He was one of the founders of the Progres Medical. He founded the Journal L’Obstetrique and, in addition, was the corresponding editor for France of the American Journal of Obstetrics and Gynecology. He was also an officer of the Legion of Honor (a very high distinction in France).
The scientific work of Budin is considerable. He enriched obstetrics and pediatrics with numerous original clinical and experimental works; one is convinced of this by glancing at his publication list (See the extensive Bibliography of Dr. Budin in the paper entitled “The Founders of Neonatology”).
The Teacher
His teaching was marvelously clear; his lectures, seminars and conferences were always meticulously prepared. A man of a great erudition, he never spoke without bringing facts and examples to strengthen his assertions. A speaker of great charm and authority, Budin captured his audience.
During discussions he in the various societies to which he belonged, he displayed the same qualities exposing his opinions with firmness and courtesy and knew how to find the right balance in controversies. Most of the time he managed to have the opposition rally with him in key disputes.
Yersin, who discovered the bacterial agent responsible for the plague, was a student of Budin. In a letter to his mother written in 1887, he expresses his feelings about his attending:” I hold Professor Budin in great esteem. Each time, we attend a delivery, the next day we have to give him a report on every event. I made a delivery last Monday. It was very funny, except for the mother. A little girl was born under my direction (…) This week I attended two interesting cases of dystocia (forceps application)”.
Family and Social Life
Pierre Budin married Marie-Therese Sasles (born November 3, 1870 at Flers, Orne). M.T. was an English teacher. She had studied at Caen in the Calvados and graduated July 11, 1889. Pierre and M.T. were engaged for 5 years, as mentioned by the long, pompous, boring blessing speech given by Bishop Patry, October 27, 1893.
She was 23; he was 47. Pierre was what the French call a “vieux garcon.” (old bachelor) The reason for this prolonged engagement was probably the young age of the bride. He loved his wife and called her “ma mignonne”. On July 19, 1896, he entered in his diary, “beautiful moon; back to Paris in a convertible buggy, the cabman does not know the way. It is so nice to breath fresh air and to feel a warm heart beating next to yours.” M.T. wrote about her husband that she loved him dearly. M.T. loved photography and wrote in a letter to her mother that she had taken pictures at the maternity. She processed her own plates and had a small laboratory in her apartment. Pierre and M.T. could not have children.
They both enjoyed high society life. They were close friends of the Rotschilds. They enjoyed theater and music as witnessed by letters of Rejanne and Monnet-Sully, famous French actors of the time. An exchange of thank you notes with Monnet-Sully about “un fauteuil” obtained at the Paris Opera or to the Theatre Antoine testified about their love for the arts. They obviouslly knew Jean Richepin, a poet and well known lecturer, as well as Lyautey, the future Marechal de France, who at that time was haunting the Parisian literary circles. Budin was very found of Tourguenief, a Russian novelist, who contributed to the diffusion of Russian literature in France. Kipling was among his favorite authors. Senators P. Strauss and Dr.Bourneville (the man who discovered the tuberous sclerosis was also a senator) were among their friends. Bourneville contributed, in fact, to the creation of the specialty of obstetrics. P. Strauss was one of the co-founders of the “ligue contre la mortalite infantile.”
During his professional life, Budin occupied successively three apartments in Paris. The first one, located on 129 Boulevard St. Germain was a very comfortable flat. After his marriage, he lived at 4 avenue Hoche, next to the Arc de Triomphe, and later moved to an hotel particulier located at 46 rue du Dr. Blanche in the middle of the 16e arrondissement, headquarters of the “haute bourgeoisie,” not far from the Bois de Boulogne. The Budin’s had four servants. In the morning, he attended patients at the hospital; in the afternoon he had a private clinic at his home. In the evening, he prepared lectures or wrote and revised papers. He was one of the first physicians in Paris to use a telephone.
In addition to his native language, Pierre Budin spoke English and German. With his wife, he travelled throughout Europe and attended the first European organized medical meetings (he mentioned in his diary a special bed made in Sweden for deliveries).
Curbing Infant Mortality 1892 -1907
Budin spent a lot of time teaching and practicing the emerging specialty of modern obstetrics, while in fact, he was also mostly pre-occupied by the future of children. “When I was service chief at the Hospital de la Charite, I took care of the newborns and I was stricken by the response made by women I had previously delivered when they came back for another pregnancy. I asked them what happened to the previous infant they gave birth to, and often they told me: He died! In fact, after discharge from the hospital, their only guide was the vague experience of grandmothers, concierges, and herbalists (pharmacists). Mixed by various biases, they had made mistakes, so their children became sick and died.”
Budin studied the basic rules of hygiene and feeding of the newborn, arguing that “the high neonatal mortality was due to the lack of follow-up, good advice and special care; the obstetricians stopped taking care of them shortly after birth, and the pediatricians were not interested in their condition until they were two years old.” (5,17).
At the Federation of French Socialist workers in 1892, he shared his vision for infant health: “A revolution took place during the last few years. Puerperal fever decimated our maternities. Today, thanks to the work following Louis Pasteur’s discoveries, women in confinement should not die anymore. In well-kept obstetrical wards, maternal death has become an exception. We may hope that a similar revolution may happen for the infants. Recent works, as a consequence of Pasteur’s research, with milk sterilization at home, have markedly decreased the high infant mortality rate. Poor and rich alike, will be able to keep their infants and experience happiness at home without the challenge of sadness. The nation and the world will benefit” (5). He also quoted President Roosevelt: “A nation losing its population is committing suicide.”
The mark of Budin to establish good infant care facilities and proper hygiene was encouraged by the government because low birth rates and infantile mortality were placing France in a dangerous situation, especially in the face of an expansionist Germany because of an insufficient population growth. Furthermore, France was actively colonizing numerous territories and stretching its manpower very thin in Asia and Africa. The French government, a young republic, understood the consequences of poor birth rate combined with high infant mortality and simultaneously launched very structured education (school became mandatory) and health programs oriented toward preservation of children. This resulted in the creation of numerous modern hospitals and maternities.
Budin, with the help of his political friends, put all his strength in launching modern obstetrics, which included infant care. Puericulture became a non-stop endeavor. Two presentations on the results of maternal education and the sterilization of milk, were made at the French Academy of Medicine with Dr. Chavane (1892-1893). At the same time, he created the first infant clinic at the hospital of La Charite, in 1892. The goal was simple: encourage breast feeding by all possible means, provide mothers with good advice, and supply the help necessary to provide the best nutrition for the infant.
One day Budin had remarkable experience; while visiting the maternity a foreign physician told him, “Your clinic is not very interesting, all the infants are doing well!” (5). This colleague had not understood the benefits of preventive medicine. However, physicians with vision adopted the Budin’s ideas, and the clinic movement spread through France to Belgium, Italy, Hungary, Canada, and Spain.
The French Committee for Children subsequently recommended more regular follow-up visits of the small infant and a law (The Roussel Law ) was promulgated to make bi-monthly clinic visits mandatory. Private and public industry both recommended the creation of infant clinics . At the Brussel’s Hygiene Meeting , Budin recommended that the government and its administrative structures survey and monitor infants’ diets. He also advocated that at each wedding and infant’s birth, a pamphlet should be given about breastfeeding.
His beautiful book The Nursling was published in 1900, followed ( with English translation in 1907 (18). In 1902, Budin and P. Strauss with the help of the philanthropist Th. Roussel, founded the “League Against Infant Mortality” (19), which emphasized concentrating efforts on preventing threats to the health of infants. Extremely good results were quickly obtained by a centralized effort rom various organizations working with a same principle. Numerous French counties reported that the infant mortality rate, which was as high as 288/1000 fell to 112/1000. How were these results obtained? By multiplying the infant clinics; improving the training of physicians, nurses and midwives; evaluating the help of the “prefets” (equivalent to our governors); and, by keeping track of the results so that constant modifications could be made.
The Sad Death of Dr. Budin 1907
In 1907, Pierre Budin was stricken with pneumonia while at a conference in Marseille. From the first day of the sudden illness he understood that the situation was critical and he gave to Dr. Perret very coherent instructions for the continuation of his work. He dictated the following letter (20), which was given after his death to his friend P. Strauss and to his students and colleagues: Maygrier, Boissard, Bar, Bonnaire, Mace, Perret, Jeannin and Devraigne:
“My dear friends,
The fate of French children rests on you. I count on you to be the first to do the necessary work to develop infant clinics and later delegate this task to your students”.
Budin.
Dr. Budin closed his eyes forever on January 22, 1907 in a hotel room in Marseille.
Marie-Therese Budin, his wife of 14 years, continued his work, and the Foundation Pierre Budin (21) was created (It later became the “Ecole de Puericulture”). A model infant clinic was opened to the public on May 24, 1909 by Emile Loubet (ex-French President).
On March 5, 1923, Marie-Therese Budin received the high distinction of the “Legion d’honneur.” In her response to Paul Strauss who placed the red ribbon around her neck she said, “Everything I did, I did for love of my Husband; then for love of infants and their mothers who are frequently admirable”.
Bibliography
- Banquet offert au Dr. Pierre Budin par ses eleves et amis a l’occasion de sa nomination de Professeur. Octave Doin, Paris 1897.
- BONNAIRE, A: Le Professeur Budin. Presse Medicale No 8, jan 26,1907.
- BUDIN, P. : Ligature du Cordon Ombilical , Progres Medical , Paris
- BUDIN, P. De la Tete du Foetus au point de vue de l’Obstetrique (Doctorate Thesis 1876)
- TOUBAS P. L. : Personal archives of Dr Pierre Budin. Private collection.
- BUDIN, P. La Ville de Paris et la Mortalite Infantile . Paris, Masson, 1904, 40p., 17 fig.
- BUDIN P. La mortalite Infantile dans les Bouches du Rhone. Obstetrique 1907; 304-45.
- BUDIN, P. Les Consultations de Nourrissons, Arch gen de Med., Paris 1905, 1, 1234-1257
- BUDIN, P : Les Consultations de Nourrissons, Ann. de Med. et Chir. inf., Paris, 1905, 618 – 645
- BUDIN, P. Des Consultations de Nourrissons, leurs resultats, V.1 Ibid 11 289 -305 Bull. Acad. de Med. Paris. 1906.
- BUDIN, P. Allaitement et Hygiene du Nourrisson. L’obstetrique, Janvier, 1906.
- BUE (V.), L’ Oeuvre de Budin en puériculture . sse méd., 107, nø 19, p. 147-148 1907
- BUDIN , P. : Le Nourrisson: alimentation et Hygiene. Enfants debiles et enfants nes a terme. 1900. Doin Ed. Paris.
- BAR (P.), Pierre Budin. Chaire de clinique obstétricale. Leçon inaugurale. Paris, Capiomont, 1908, 55 p.
- MAUREL (P.), Les Prs de clinique de la Faculté de médecine de Paris. Paris, Steinheil, 1907, p. 57-61 – C 760
- MOLLARET HH, BROSSOLET J. Alexandre Yersin ou le vainqueur de la peste, Paris: Fayard ed. 1985; p 321.
- BUDIN, P. L’Allaitement Paris. Lecrosnier er Babe, 1892, 23p, 10 fig.
- BUDIN , P.: The Nursling . London. Caxton Publishing Co.,1907.
- Ligue contre la mortalité infantile. La Revue philanthropique, 1907, p. 251-263
- GAUTIER (A.), Décés de Pierre Budin. Bull. Académie de médecine, 1907, nø 5, p. 163-166
- Statuts de la Fondation Pierre Budin. Paris, Doin ed. 1911
The First Neonatologist – the first neonatologist was a midwife:
Madame Henry and the incubators of Dr. Tarnier
by Paul. L. Toubas (University of Oklahoma, Health Sciences Center at Oklahoma City) and R.A. Nelson (University of Kansas at Wichita)
On 13th of July 1881, at the time of my appointment as midwife-in-chief at the Maternity, Pr. Tarnier, during myvisit of the various services of the hospital, brought me up to date on the improvements and changes which he had obtained and those he was planning. He showed me in the wet nurse room, called the “crèche”, an incubator that he had arranged to be built. He explained the mechanism and told me the advantages which would benefit the infants born prematurely or feeble and asked me to help in his research and to start again the experiments he had done in the past. Everybody, today recognizes, not only the inocuousness of the incubator, but also the excellent results they are giving.
It was not the same in 1881; at that time, it was good to prove that a living individual was able to continue living in that device. The first infant was placed in an incubator almost dying; He was, thanks to the device been resuscitated, and survived. This first trial was a success, other infants were subsequently placed in it and survived.
These successes were soon recognized, not only in the medical word, but also in the lay public. The press took over the topic. From the point of view of the discovery and the services it was able to render, this publicity was excellent, but it produced, very quickly a dilemma. We were often brought infants born in the city; but we had only six incubators and five wet nurses; this was barely sufficient to accommodate the sick infants of the ” Maternity”. As it was impossible not to admit these infants at the nursery of the hospital, our service was soon overloaded.
To remedy this inconvenience, there was only one means, to create a special service. I talked to Mr. Tarnier: he supported and encouraged me a lot, but in order to realize this project, money was needed. I tried to establish a society which we called ” L’Oeuvre des couveuses”. It brought me with relative ease, subscriptions and few donations, about 10,000 Francs; this was insufficient. I searched out Mr. Peyron, Director general of ” Assistance Publique”; I told him about the logistic difficulties of the service of the crèche, he listened receptively, understood the importance of the foundation which I was soliciting, asking me to write everything that I told him, adding:” Find a little bit more money and we will help you.”- I then approached the Municipal Council of the city of Paris. Mr. Paul Strauss agreed to study the question and to present it to the Council. Mr. Peyron was consulted and gave a favorable advice, and in 1891, the establishment of the service was voted; a sum of 40,000 Francs, taken on the pari mutual betting was awarded.
The design of Mr. Rochet, architect of the Assistance Publique was adopted. It was decided that the pavilion will be constructed with masonry tiles. Mr. Imard (retired architect and inspector of the Assistance Publique) agreed to help us with its advice. When the pavilion was finished the costs exceeded by 17,000 Francs the initial project. The Council agreed to pay the difference.
Mr. Peyron, general director, Mr. Rousselle, president of the municipal council and Dr. Dubrisay, came to visit the new construction. They liked the inside, but disliked the grayish and sad exterior. To brake the monotony of the masonry tile , we ordered the application of lattices painted in green on which plants could entwine. The 10,000 Francs I had collected helped to pay for the heating system and other devices that the administration was not able to provide; in addition 14 incubators were built on the model designed by Mr. Tarnier with few additional modifications; finally we purchased an autoclave and everything needed to embellish the pavilion inside and outside. On July 20th 1893, the pavilion was open. I had the good fortune to direct the pavilion, to obtain the help of Mrs. Bataille, who combined the three qualities indispensable to all who must direct an hospital service: goodness, professional honesty and devotion. Thus the service functioned very well. There were never complaints on the part of the public nor any reproaches from the administration.
Unfortunately, for personal reasons, I was obliged to give my resignation and to leave the Maternity, abandoning thus the service which I had so much pleasure to create.
I left the hospital at the end of June 1895, but the pavilion of the weaklings was passed into other hands, but I did not take care of it any more and closed my statistics at the end of January 1 1895.
From July 20 1893 to January I 1895, we have received on the service of weaklings 721 infants; 364 were discharged in good shape and 357 died. Among these 357, 24 were born before viability. Fifteen had grave malformations, 68 were dying and died within 24 hours after their admission to the pavilion, a total of 107 infants. We believe , we need to exclude them in order to make a correct percentage. Therefore we are going to say: Of 614 infants, we had 250 deaths. We accepted all the infants that were brought to us., weaklings born prematurely or at term, and those , who, poorly fed , needed a good wet-nurse. We also admitted infants born before viability, not only to leave hope to the parents, but also to see if we would be able to take care of infants born at less than six months of gestation.
We had made an observation of an infant born at 5.5 months gestation , weighing 780 grams; he survived 13 days, he was able to suck a little and digested fairly well. Unfortunately he died of a cyanotic spell.
Between these to dates: July 20, 1893 and January 1, 1895, we have received 74 infants, in very poor condition, having been fed artificially.
Thirtty-eight times, we noted on the observation that the milk had been sterilized, 36 times this was not indicated.
Of these 38 infants fed with sterilized cow’s milk, 15 died, thus 39.4%.
Of the 36 observations without indication of the sterilization of milk, 16 died, thus 44 percent. Combining the 74 observations of infants artificially fed, we found 31 deaths, thus 41%.
What is the disease which would give a comparable statistic?
All these infants died of enteritis and similar infections; however a proportion of them came from hospital services were that mode of feeding was part of the feeding protocol and probably properly carried out.
When you have observed the agony of these little creatures, you wonder why this type of feeding is still advertised.
Already, in 1883, Mr. Tarnier had us sterilized the milk which was given to infants born at the Maternity. This milk was placed in an American cooker. To carry it at more than 100 degrees Celsius, he made us use oil , the water supplemented with sodium chloride. He hoped to insure complete sterilization of the milk.
In this manner, we tested sterilized milk undiluted with one-third or one-half water, and finally milk sterilized with unsalted beef broth in equal parts.
The American cookers remained one hour in the boiling liquid. When the lid was raised, there was no cream on the milk. It was immediately poured in small glass bottles containing 50 to 60 grams which served to feed the infants.
With these different preparations, we have nourished a certain number of infants. With some of them , we have been able to continue artificial feeding up to two weeks or more. The condition of the infant has always caused us to interrupt the feeding momentarily or definitively, to replace it by breast feeding direct, or gavage, either because the infant was loosing weight or had too much diarrhea.
All these observations have been controlled by Mr. Tarnier; on each page of the chart we have noted the preparation used, the number and the hours of feeding, the quantity of milk taken in 24 hours, the condition of the infant, his temperature in the morning and the evening, the number and the appearance of the stools. For 90 of these observations, I copied , every day, with water color the color of the stools. All these water colors were also seen by Dr. Tarnier, who compared them to the to the diaper of the infant. You will find a specimen along with that study.
Every morning and evenings, the infant under observation was weighted; the graphic tracing is very interesting. In direct feeding by a mercenary wet-nurse, 5 or 6 days after birth, the infant had regain his initial weight. If he is fed by his mother, specially if she is feeding for the first time, this weight is only gained around the ninth or tenth day.
With artificial feeding, it is rare that it rare that weight is regained at that time.
All the research that we have done brought us to the conclusion that artificial feeding was particularly dangerous during the two months following birth. We are convince that it is wrong to believe that sterilization of cow’s milk avoid all these dangers. In infants fed that way , we have seen often green diarrhea and we have always been surprised by the foul smell of the diapers and vomiting; we have most of the time observed abdominal distention and persistent erythema. In the mixed feedings, the prognosis is more favorable, this mode of feeding, if breast feedings periods are more numerous, succeeds well. In that case the milk and the unsalted broth (1) sterilized together (10, 20 30 grams before breast feeding) gave us relatively good results in the newly born infant. On 62 infants fed in that fashion, 59 were discharged in good condition, 3 died.
Mr. Michel, resident of Mr. Prunier, pharmacist of the Maternity, did in 1894 some experiments on the artificial digestion of milk. We gave him two samples; one of pure sterilized cow’s milk, the other of milk and unsalted broth, diluted 50% and sterilized. He did not know the content of the two bottles, they were only identified by bottle Nr. 1 and bottle Nr. 2. Here are the results he obtained.
Artificial digestion of two milk samples given to Mr. Michel on January 8 1894.
Experiment 1
sample size... 100mL
addition of ... 0.50 gm HCl.
1 gm of amyloid pepsin from the Codex.
Digestion: about three hours at 40°C.
10 ml of each such treated samples are evaporated at 100°C. ( after filtration) until complete desiccation.
The Nr. 1 sample (pure sterilized milk) leaves 0.719 of dry residue containing peptones and the soluble materials of the milk.
The Nr. 2 (milk and broth sterilized) leaves 0.616 gm of residue. The two samples were sterilized with the autoclave.
Experiment 2
In the same conditions as the first, but the duration of the digestion was 4 hours. The Nr 1 sample left 0.875 gm of residue, the Nr. 2 left 0.750 of residue.
These two assays are in agreement to demonstrate the superiority of Nr. 2 on the amount of principal components held in dissolution. Did these components preexisted in the milk of were they the product of digestion?
New experiments are necessary to take into account additions made to the milk.
REMARKS AND OBSERVATIONS DONE AT THE PAVILION OF THE FEEBLE.
Some diseases are more frequent in prematurely born infants or weaklings than others. Those we have most commonly observed at the nursery of the maternity included some diseases of the respiratory and digestive tube.
These diseases are well known, except two , perhaps which still are not, we believe, completely studied. The first which we are going to talk about is an non syphilitic affection of the nasal fossa. It is relatively frequent in feeble infants and must show: 1) the difficulty which they have with swallowing 2) the ease with which they vomit. In these two cases, they frequently reject milk through the nose; a little bit of this milk stays in the upper part of the pharynx and the posterior part of the nasal fossa mixing itself with secretions, alters itself and ferments quickly. Mucous membranes, on which it is deposited are irritated and inflamed. One sees then coming from the nares a purulent discharge; if one is unable to disinfect these a focal areas, the tissues change more and more, the skeleton of the noses is deformed, flattens, the nasal bridge gets depressed, the shape of the nose appears to be changed like if it was broken. The nose will keep forever this shape. It is deformed as it is in syphilitic ozena.
All these little patients do not heal; a certain number dye of cyanotic spells or broncho-pneumonia and present some days before their death a swelling of the upper lip and the tissues of the face. At autopsy, one finds the nasal fossa filled with putrid material, with underneath ulcerations of the nasal mucosa. Nothing , after cut of the brain, resembles syphilitic lesions.
Nasal lavages are indicated, but this is difficult to do. We use cotton soaked in boric water and inserted as far as possible. We also apply Vaseline mentholated or borated. At the moment I left the Maternity, I wanted to make an instrument to insert more deeply the small tampons. My departure made me abandon the project.
Other infants, affected in the same way, die , we have said of broncho-pneumonia. This infection, well localized in the posterior region of the nasal fossa, may invade other organs and produce deadly complications. On the point of view of repercussions of localized infections influencing the general health of the infant, this disease may be compared to ophtalmia of the newborn.
We have made a review of last disease and we found 45 cases of ophtalmia that 15 died of pneumonia, or seizure without appreciable meningitis.
In newborn infants, germs are able to penetrate easily by five ways: the eyes, the nose, the mouth, the navel and ears (this fifth entry was reported by Dr. Pinard.)
Therefore all these areas should be the object of attentive surveillance, specially during the first fifteen days following birth. Because some infants may have only light infections, in some others , it may be quite severe. These occurences could be localized, either because the infant is in a better state of defense or that through appropriate treatment, the diffusion of the disease can be prevented. But in other cases the infection spreads, reaching the neighboring organs and leading to lethal complications.
We have sometimes observed metastatic abscesses from other causes, except, that a mild infection of the regions we have described.
Among the infections of the respiratory apparatus, there is one which is difficult to appreciate. We want to speak of the cyanotic spells which one notes so often in the premature infant which is not accompanied with auscultation signs and it which at autopsy one finds nothing in the lungs to explain this. This cyanosis of the newborn we believe depends on two causes, one of neurological origin and the other mechanical.
Neurological origin.- With this cause, the apneic spell originates without preludes; the infant , in his incubator or in his cradle is of a pink more or less bright color, breathing regularly, appears to be sleeping, then suddenly stops to breathe; his color becomes gray, then blue, then near black. If one is not able to give him artificial breathing, he dies.
We believe that we can attribute to this cause the demise of infants found dead in their bed.
Prognosis.- It is very serious; however, we have seen certain number of infants heal despite many cyanotic spells.
Treatment.- During the spell, insufflation and skin stimulation. Warm baths, frictions of alcohol are sufficient. Under the influence of these treatments, one sees little by little the respiration become regular and the child regains color.
In the intervals of the spells, it is necessary to give close observation to the little sick one. Do not over feed the infant. In these cases we have found advantageous to give some hot rum, one or two tea spoon before the feeding; we successfully used ozone and oxygen inhalation (see the thesis of Dr. Patel 1895) and subcutaneous injections of testicular liquid, two injections a day of 10 drops each. In 20 infants, receiving these injections, 13 were discharged in good health and 7 died.
Cyanosis of Mechanical cause.- The apneic spells in these cases are due: to abnormal development of the stomach and or the intestines. These organs, too, compressed in the abdominal cavity, push the diaphragm and impede diaphragmatic movements and diminish the capacity of the thoracic cavity.
This condition is observed in overfed infants and often in those who are nursed with a milk specially rich in casein like that is seen in artificially fed infants.
In that case, we have seen the suffocation spells after abundant vomiting in which often one can find more or less large clots of casein.
The look of the infant has no resemblence to the one we have described in cyanosis of neurologic origin. With that latter condition spells are also observed, but he is not flaccid. In general after the vomiting, the spells stops, the child returns to pink. The prognosis is grave but but less grave than that of cyanosis of neurologic origin.
Treatment.- The treatment of the spells consist of artificial respiration of the infant. But in that case, we believe that tractions of the tongue are better than insufflations; stimulation of the skin may be of great help. In the interval of the spells , treat the digestive problems and change the feedings of the child.
Each time that a difficult case present in the pavilion of the feeble, Mr. Gueniot, Surgeon in Chief of the maternity and Mr. Labadie Lagrave, physician of the hospital, gave us a generous help with their advice and we owe them a great part of the success that we have had in the service. We ask them to receive our sincere thanks.
The Engineer and the Newborns – the incubators of Mr. Lion
by W. A. Nelson M.D. (University of Kansas, Wichita) and P. L. Toubas M.D. (University of Oklahoma Health Sciences Center, Oklahoma City)
Mr. Alexander Lion, an ingenious French engineer, was the son of an inventor. The cufflinks that his father invented were patented. Nobody knows how Alexander Lion came to design an incubator for eggs, equipped with an electro-automatic thermostat. The patent was registered in Marseilles on October 28, 1889 (1). The patent established June 26, 1890 was valid for 15 years.
The incubator described by Lion in the handwritten manuscript was a big machine since five thousand eggs could be incubated at once. The device was very ingenious for its time and included multiple thermometers to insure an homogenous temperature. When the apparatus reached the appropriate temperature, an electric bell sounded and automatically adjusted the admission of gas. Lion mentioned that his incubator could function with alcohol, petroleum and other combustible substances. He guaranteed that 97% of the eggs would hatch. A sponge suspended in the incubator provided the appropriate humidity.
In the same document, Lion mentioned that “the incubator may be applied to preserve maternal heat for infants born before term (fig. 1). I tried it successfully at home on an infant born at six months of gestation. Without it, the infant would have died. This represents a new application of my system to infants born before term and to weaklings who need regular, constant and uniform heat to survive.”
Other types of incubators had previously been described to be used for weaklings, among them the Tarnier-Auvard incubator, a very simple system designed in 1885, functioning with hot water bottles. The problem with these rudimentary boxes was their unstable source of heat: “exposing the infants to the risk of burns and hypothermia” (2). Pierre Budin, the creator of the first nursery for premature infants, however, did not share this opinion. Despite their obvious technological advances, the Lion incubators were energy source dependent. In his handbook of practical nursing (3), Budin, after describing the advantages of the wood and glass incubator, explains the problems involved with the Lion system: “The Lion incubator siphons the air from the environment. This air, heated by gas, circulates around the infant. This device requires a complex system of pipes for air and gas. The high cost cannot be borne by many families. At the Maternity, we had to remove infants often from this type of incubator. The coldest season of the year is winter. Nights are very long. The gas consumption increases massively at this time of the year. Since the air is colder, it takes more gas to heat the incubator. At the end of the night, the gas pressure is very low and insufficient to heat the incubator; the temperature of the infant cannot be maintained.”
After missing his Parisian debut in the very modern maternity of Dr. Budin because of the unstable gas pressure in Paris, the Lion incubator found a stable home in the south of France in the city of Nice. This pleasant town, located on the French Riviera, enjoys a mild winter. Citrus fruits grew in the gardens of the casino. Big hotels were built fast and the economic boom brought by tourism created the appropriate environment for the establishment in 1891 of the Oeuvre Maternelle des Couveuses d’Enfants. Dr. Ciaudo, physician inspector of facilities for the protection of infants of the city of Nice, exposed the results obtained in this maternity from 1891 to 1894 (4). One hundred and eighty-five premature infants were placed in the incubators with a weight ranging from 800 to 2900 GM. The surprisingly good outcome was encouraging since 133 infants survived in good condition; 48 infants died, among them were eight infants weighing less than 1000 GM. The survival rate was 72%. According to Dr. Ciaudo, “the type of incubator used in Nice appears to be very advanced; heat is provided by an ordinary oil or petroleum lamp. The heat is constantly maintained at 37°C. An electric regulator provides an automatic regulation of the temperature.”
In the Fall of 1896, the Lion incubator made a comeback to Paris. An anonymous letter published in Pediatrics (5) describes the event: “The latest attraction of the Paris boulevards is an exhibition of an improved system of incubators which have recently been introduced to the capital, after a trial of several years by a philanthropic society of Nice. The premises occupied by this new hospital for premature infants consist of a shop on the ground floor, and its dependencies and the public are admitted on the payment of a small fee, which goes paying towards the general expanses.” Fig. 2
The Lion incubator was presented at the National Swiss Fair in Geneva. The report in 1896 to the Geneva Medical Society by Dr. Maillard was very favorable (2). Twenty-two infants were treated, fourteen survived. In his comments, Dr. Maillard shows his preference for incubators at home rather than in a special maternity. The reason was the high risk of bacterial contamination of premature infants by infected infants. The other reason was the need for breast milk to feed the premature infant. Cow’s milk at this period was frequently contaminated and a high source of infant mortality. Dr. Maillard mentions that the incubator functions appropriately on gas. Dr. Maillard, at the end of his report, adds: “This incubator (the Lion incubator) is an indispensable instrument…it will render the previous heavy wood and glass incubator obsolete (the Tarnier incubator)…only the archives of maternities could tell us how many infants have been burned or frozen by the antique system of pushing hot bottles in a wooden box!” This message announced the arrival of the technology of the 20th century in the care of premature infants.
Last Updated on 01/29/25