Pulse Oximetry
The journey to today’s indispensable, reliable, highly portable pulse oximeters began with the discovery of the blood’s oxygen-carrying properties. In 1862, Felix Hoppe-Seyler identified hemoglobin as the vital protein for oxygen transport and observed that it changed color when mixed with oxygen. In 1864 a physicist, George Gabriel Stokes, was the first to report the effect of treating blood with a reducing agent, observing that the two distinct bands merge to a broader absorption band with a peak roughly half-way between the peaks for the untreated blood. When he reintroduced oxygen by shaking the blood with air, and the original bands reappeared.
A decade later, in 1874, Karl von Vierordt demonstrated that light transmission through the human hand changed when blood flow was restricted — the first evidence that light could be used to probe blood oxygenation non-invasively. By 1939, German scientist Karl Matthes developed the first two-wavelength oximeter. Although it used red and infrared filters to track saturation, it was cumbersome and required frequent, manual calibration, limiting its use to the research laboratory.
World War II catalyzed a shift toward clinical application. Military aviators frequently suffered from “silent” hypoxia at high altitudes, leading to fatal crashes. In 1942, Glenn Allan Millikan developed lightweight ear-piece oximeter for pilots and coined the term “oximeter.” According to a report by his wife, it could be used to control a servo system that would control the supply of oxygen to the mask of the pilot wearing the device. These early devices struggled to distinguish between arterial blood and the surrounding tissue. In 1940, J.R. Squire discovered that “blanching” the tissue with pressure could help isolate the blood signal, a technique that remained standard for decades.
During the 1960s, Hewlett-Packard released an 8-wavelength ear oximeter. While highly accurate, it was massive, cost roughly $13,000, and could cause skin burns due to the heat required to “arterialize” the blood in the earlobe.
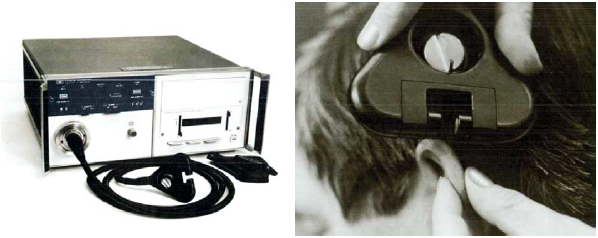
The most significant leap in the field occurred not in a hospital, but in the laboratory of Takuo Aoyagi, an electrical engineer at Nihon Kohden in Japan. While attempting to improve a device for measuring cardiac output, Aoyagi noticed “noise” caused by the patient’s pulse. He realized this noise was actually the signal he needed: it was the only part of the light absorption that changed with the heartbeat, meaning it represented arterial blood alone. By focusing on the change in light absorption during a pulse (the “Ratio of Ratios”), he could ignore the static absorption of bone, skin, and venous blood. Nihon Kohden applied for the first pulse oximetry patent in 1974.


Despite the invention in 1974, it took a series of landmark studies in the 1980s to prove that pulse oximetry was essential for patient safety. Studies by Jeffrey Cooper and R.L. Knill in 1982 proved that clinicians could not visually detect hypoxia until a patient was in a critical state (often below 80% saturation). In 1988, Charles Coté showed that “blinded” clinicians (those who couldn’t see the oximeter screen) missed significant desaturation events in children, proving the device was a necessary early-warning system.
In 1986, the American Society of Anesthesiologists (ASA) formally encouraged its use; by 1989, pulse oximetry became a mandatory standard of care for every patient undergoing anesthesia. In 1993, the Moller Study of 20,802 patients confirmed that pulse oximetry increased the detection of hypoxia 19-fold, solidifying its global adoption.
During the 1990s, the technology evolved from a fragile tabletop monitor into a robust digital tool. Early monitors failed if a patient moved. In the 1990s and early 2000s, companies like Masimo developed Signal Extraction Technology (SET), using complex algorithms to “read through” motion and low perfusion. Modern medical-grade pulse oximeters are compact, reliable, portable, and non-invasive, and widely deployed throughout hospitals as well as in operating rooms, while inexpensive over-the-counter oximeters are integrated into wearables and smartphones.


Most importantly for care of sick and premature newborns, pulse oximetry is the standard, non-invasive method for monitoring a baby’s arterial oxygen saturation and responding rapidly to changes, reducing the risks of hypoxia or hyperoxia. It is also now a standard of practice for screening newborns for congenital heart disease.
Comparison: 1980s Pioneers vs Modern Smart Oximeters
| Feature | 1980s First-Generation (e.g., Nellcor N-100) | Modern “Smart” Oximeters (2020s) |
| Size & Portability | Large, heavy tabletop units; required AC power. | Pocket-sized or wearable; battery-powered for days/weeks. |
| Motion Tolerance | Very Poor. Movement caused “false alarms” or signal loss. | High. Advanced algorithms (like Masimo SET) filter out motion noise. |
| Low Perfusion | Failed if the patient was cold or had low blood pressure. | Accurate even in patients with “weak” pulses or shock. |
| Signal Processing | Basic “Ratio of Ratios” linear calculation. | Discrete Saturation Transform (DST) and AI-driven filtering. |
| Data Output | Numeric $SpO_2$ and heart rate only. | Plethysmograph, Perfusion Index (PI), and Respiratory Rate (RRp). |
| Connectivity | None (paper charts or manual recording). | Bluetooth/Wi-Fi; syncs to EHR (Epic/Cerner) and smartphones. |
| Sensor Type | Bulky, reusable clips or taped rubber probes. | Disposable “wraps,” soft-silicone clips, or wrist-worn rings. |
Historical TImeline
| Year | Milestone |
| 1864 | Hemoglobin identified as the oxygen carrier. |
| 1935 | First two-wavelength oximeter developed by Karl Matthes. |
| 1942 | Glenn Millikan coins the term “oximeter” for his aviator ear-piece. |
| 1972 | Takuo Aoyagi discovers the “Ratio of Ratios” principle using the pulse. |
| 1974 | Nihon Kohden applies for the first pulse oximeter patent. |
| 1981 | Biox and Nellcor bring refined pulse oximeters to the US market. |
| 1986 | Pulse oximetry becomes a standard of care in US anesthesiology. |
| 1993 | The Moller Study confirms a 19-fold increase in hypoxia detection. |
| 2020s | Wearable “smart” oximeters allow for remote patient monitoring. |
Further Reading
- The History of Pulse Oximetry Measurement, by Curious Cyboard, https://curiouscyborg.com/the-history-of-pulse-oximetry-measurement/
- Zacharis DK, Zhao DZ, Ganti L: “”History and Social Implications of the Pulse Oximeter.” Cureus 16(8): e68250. DOI 10.7759/cureus.68250
- Quaresima V, Ferrari M, Scholkmann F: “Ninety Years of Pulse Oximetry: History, Current Status, and Outlook.” Journal of Biomedical Optics 29(S3). August 2024.
- Magwenzi MM: 8036 From past to present: the evolution of pulse oximetry and its transformative impact on paediatric medicine. Archives of Disease in Childhood 2025;110:A115.
- AAP Guideline on Newborn Screening for Congenital Heart Disease with Pulse Oximetry, 2011, updated 2025.
- Obituary, Dr. Tokuo Aoyagi, New York Times, May 1, 2020.
Last Updated on 02/20/26